Human Rights, key Populations and Gender
Background
UNDP’s work in health and development -- elaborated in UNDP’s HIV and Health 2022-2025 Strategy -- is guided by respect for and promotion of human rights and gender equality as set out in the United Nations Charter, the Universal Declaration of Human Rights and other international treaties. In the context of HIV, tuberculosis and malaria, there is strong recognition of the need for greater attention to key and other vulnerable populations in all epidemic settings, including action to address social, legal and cultural barriers to access HIV and other health services, promotion of human rights and rights-based approaches, and support for engagement of key and other vulnerable populations in policy development, health governance and programming.
Likewise, the Global Fund’s 2023-2028 Strategy includes the imperative to maximize health equity, gender equality and human rights by deepening the integration of these dimensions into HIV, TB and malaria interventions, including through expanding the use of data to identify and respond to inequities, scaling up comprehensive programmes to remove human rights and gender-related barriers, and leveraging the Global Fund’s voice to challenge harmful laws, policies and practices. Furthermore, growing inequalities and pervasive human rights, gender-related and other structural barriers continue to exacerbate vulnerability to HIV, TB and Malaria infections and limit access to services. The failure to put communities at the centre of the design, implementation and oversight of programmes has resulted in suboptimal programming and health outcomes.
A growing body of evidence suggests that human rights barriers can drive people – in particular, key populations1 away from health-seeking behaviour, thereby fuelling the spread of the three diseases. These barriers can include, among others, stigma and discrimination, punitive legal and policy frameworks (e.g. but not only criminalization), lack of informed consent, mandatory or coerced testing, and gender-based violence. As a result of gender-based discrimination, women and girls are disadvantaged when it comes to negotiating safer sex and accessing HIV prevention information and services. However, despite recognition of this reality and substantive guidance on the importance of programmes to combat human rights and gender-related barriers, a Global Fund analysis found that many grants do not include this programming, or, if they do, it is included at very low levels.
In light of the above, applicants are expected to include:
- an assessment of the human rights related barriers in their country, including stigma, discrimination, and violence against key and vulnerable populations. They are also asked to consider existing legal and policy settings and contexts, as well as age-specific barriers, including lack of independent access to HIV and/or sexual productive services.
- an assessment of gender related barriers which considers gender inequalities and barriers, why they exist, and their impact on health outcomes. Applicants should consider how gender intersects with other barriers, such as age, place of residence, race/ethnicity, occupation, gender/sex, religion, education, socioeconomic status and social capital.
For both assessments, applicants are asked to include which barriers will be addressed with GF financing and expected outcomes. If an existing assessment is available (such as one completed as part of a National Strategic Plan review), it should be attached. If not, applicants are requested to complete one.
Objectives of this section
This section of the Manual includes links to the existing and substantial policy and programming guidance, as well as practice pointers to implement programmes to address human right barriers and promote gender equality at various points in the grant life cycle. It is not meant to be an exhaustive section of the guidance and resources available, but rather a guide to help programme and policy staff to develop, implement and evaluate programmes that seek to promote an enabling environment with a focus on key populations.
A key goal of this section is to facilitate an understanding of human rights, the needs and vulnerabilities of key populations and women and girls, and the interrelatedness of these areas in the context of achieving positive health outcomes for HIV, TB and malaria, and to prepare Country Offices (COs) to advocate for, and effectively implement and evaluate, programmes to promote and protect human rights and gender equality. Recognizing that these are issues which can often be misunderstood or deprioritized in funding request and in grant budgets, it is strongly recommended that relevant Project Management Unit (PMU) staff closely consult with their contact in the UNDP Global Fund Partnership and Health Systems Team (GFPHST) to answer any questions, provide guidance, and to ensure that they have access to the most up to date policies and resources. To support the introduction of this work, the HIV and Health Group (HHG) has developed a vetted roster of qualified consultants who can help with policy and programme work to support design, implementation or evaluation of human rights, key populations and gender interventions.
Sustainable Development Goals
The 2030 Agenda for Sustainable Development (2030 Agenda) reflects and responds to the increasing complexity and interconnectedness of health and development, including widening economic and social inequalities, rapid urbanization, threats to climate and the environment, pervasive gender inequalities, the continuing burden of HIV and other infectious diseases and the emergence of new health challenges, such as the growing burden of non-communicable diseases (NCDs). Universality, sustainability and ensuring that no one is left behind are hallmarks of the 2030 Agenda.
The Sustainable Development Goals (SDGs) recognize that many areas of development impact health or an important health dimension and that multisectoral, rights-based and gender-sensitive approaches are essential to addressing health-related development challenges.
Human Rights
Evidence shows that human rights barriers can impede the access to and uptake of critical HIV, TB and malaria prevention, treatment and care services. In the context of HIV, these barriers can include punitive legal or policy environments that criminalize, or otherwise punish, key populations; widespread stigma and discrimination; and lack of informed consent or medical confidentiality. High levels of human rights violations and discrimination against members of key populations increase their vulnerability to HIV and deter access to HIV prevention, treatment, care and support services. Laws that criminalize or otherwise punish the behaviour of key populations, as in the case of men who have sex with men (MSM), male/female/transgender sex workers (SW), people who use drugs (PWUD), or transgender people, present additional barriers to access to services.
People in prison, or other closed settings, can also be negatively impacted by punitive norms that hinder their access to services (e.g., gender insensitive conditions, ban on harm reduction services, lack of access to condoms and Pre-exposure prophylaxis (PrEP). People living with TB —a disease associated with poverty and social inequality that particularly affects vulnerable populations with poor access to basic services— can experience high levels of stigma and discrimination or unnecessary and mandatory hospitalization that deviates from the WHO guidelines, unavailability of TB prevention and treatment services in prisons, or lack of access to TB services (for instance, for migrant workers).
Less is known about the intersection of human rights and malaria. However, malaria is also linked to poverty, with migrants, refugees, rural populations, prisoners, and indigenous populations experiencing high rates of infection. Social inequality and political marginalization may impede access to health services, and additional barriers may be created by language, culture, poor sanitation lack of access to health information, lack of informed consent in testing and treatment, and inability to pay for medical services.
Table 1: The table below highlights the possible legal and policy environment’s impact on the number of people infected with HIV.
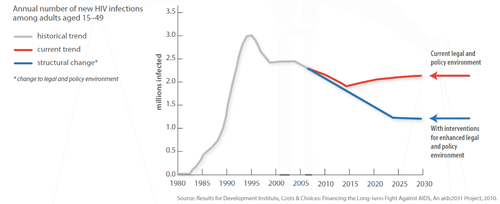
This fact sheet includes examples of how laws and practices can obstruct the HIV response and waste resources for support treatment and prevention efforts, as well as potential positive outcomes when good practices and laws based on human rights and available evidence are enforced.
Promoting and protecting rights in the context of HIV and TB is critical to ensuring that investments in national responses are fully realized.
Key Populations
Key populations in the health response are populations that are often subject to discrimination, criminalization and human rights abuses, thereby severely limiting their ability to access health services. In some settings and populations, such as in prisons and among some migrant and displaced populations, risks of HIV, TB, malaria and other diseases are also high, while access to services is frequently poor. There is now strong recognition that major epidemics cannot be ended without greater attention to key populations in all epidemic settings. This includes addressing social, legal and cultural barriers to accessing HIV and other health services, and consistent inclusion and participation by key populations in policy development, health governance and programming.
HIV: Key populations include men who have sex with men, sex workers, people who inject drugs, transgender people, people in prisons and other closed settings, and their partners. People living with HIV are also part of the key populations. In 2023 1, median HIV prevalence among the adult population (ages 15–49) was 0.8% globally. However, because of marginalization, discrimination and in some cases criminalization, median prevalence was higher among certain groups of people.
- 2.3% higher among young women and girls aged between 15 and 24 in eastern and southern Africa
- 7.7% higher among gay men and other men who have sex with men
- 3% higher among sex workers
- 5% higher among people who inject drugs
- 9.2% higher among transgender people
- 1.3% higher among people in prisons.
- The risk of acquiring HIV is:
- 35 times higher among people who inject drugs than adults who do not inject drugs.
- 30 times higher for female sex workers than adult women of the general population.
- 28 times higher among gay and bisexual men and other men who have sex with men than adult men of the general population.
- 14 times higher for transgender women than adult cisgender women of the general population.
TB: Key populations may include people in prison and people in other closed settings, people living with HIV, migrants, refugees and indigenous populations.
Malaria: While the concept of key populations in the malaria response is relatively new, and less understood than for HIV or TB, refugees, migrants, internally displaced people and indigenous populations are all at greater risk of malaria transmission, as they have decreased access to care and are often marginalized.
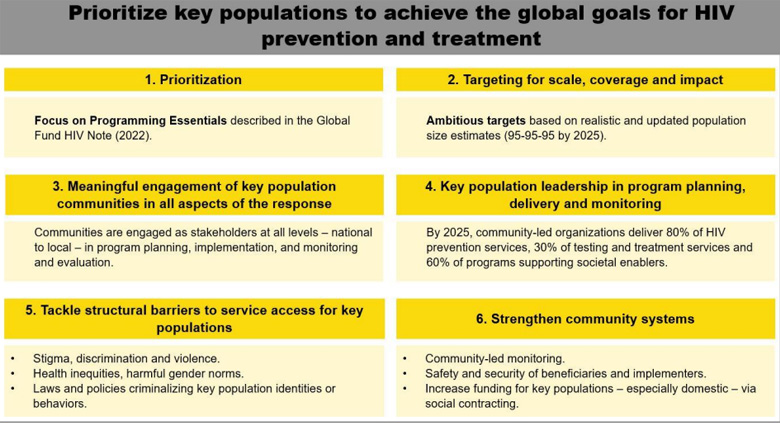
The Global Fund’s technical Brief HIV Programming at Scale for and with Key Populations describes the essential interventions and approaches for key populations that should be incorporated in HIV funding requests. It is based on the latest normative and implementation guidance, including the World Health Organization (WHO) Consolidated Guidelines on HIV, Viral Hepatitis and STI Prevention, Diagnosis, Treatment and Care for Key Populations (2022) and other guidance documents.
When preparing funding requests and interventions to meet the needs of key populations, Country Offices are strongly encouraged to review the technical brief guidance in detail. This Introduction outlines why key populations are especially vulnerable to HIV. Section 2 examines the HIV Program Essentials and the prioritized interventions in the HIV Information Note, provides details relevant to key populations, and considers service delivery approaches. Section 3 shows how to incorporate key population interventions into Global Fund proposals. It is structured around three of the Global Fund Strategy’s objectives: 1) maximizing people-centred integrated systems for health, 2) maximizing the engagement and leadership of most-affected communities (including key populations), and 3) maximizing health equity, gender equality and human rights.
Key messages from the technical brief:
Gender
HIV: Adolescent girls and young women aged 15–24 years are at particularly high risk of HIV infection. Gender inequality has direct implications for women’s and girls’ risks of acquiring HIV. Women and girls account for 48 percent of new HIV infections worldwide and 59 percent of new infections in sub-Saharan Africa, and AIDS remains one of the leading causes of death for women aged 15–49 years globally.
Harmful gender norms and inequalities, insufficient access to education and sexual and reproductive health services, poverty, food insecurity and violence, are at the root of this increased HIV risk for young women and adolescent girls. Gender-based violence has significant implications for women’s and girls’ risks of acquiring HIV and impairs their ability to cope with the virus. Gender inequalities and norms also substantially increase the risks faced by women and girls who belong to other key populations. In low- and middle-income countries worldwide it is estimated that female sex workers are more than 13 times more likely than the general population to be HIV-positive. Transgender women are particularly vulnerable to HIV, having almost 50 times the odds of having HIV than the general population worldwide. Similarly, women who inject drugs are at higher risk of HIV compared to men who use drugs. As mentioned above, these key populations are also criminalized, creating further barriers to accessing health services. TB and HIV co-infection also increases women’s health risks. Women from these key populations living with HIV are highly susceptible to developing active TB during pregnancy or soon after delivery, making TB a leading cause of death during pregnancy and delivery, and thereafter.
TB: Gender analysis and gender-responsive programming is comparatively new to the field of TB. Considerable debate on the gender divide in TB persists at all levels: medical research is divided on the ways in which TB symptoms in men and women differ, and there is inadequate medical data on women’s experience of TB in particular. The impact of TB on pregnancy is under-researched. Environmental contributions to women’s and men’s TB infection rates are ill understood. Studies of women’s and men’s differential access to TB health services have produced a range of contradictory findings, with little consensus on whether or not gender barriers to TB services access exist, and incomplete explanations for those gender differences that have been identified.
Malaria: Evidence indicates that malaria transmission is determined in large part by social, economic and cultural factors that intersect with sex-specific and gender-specific vulnerabilities. These vulnerabilities are largely still under-researched and not considered in programmatic responses. Gaps in our understanding are important to explore further, as they address deeper gender inequalities, and interventions that address the structural drivers of the disease are likely to be more effective and sustainable. Investment to address the social determinants of malaria has the potential to significantly move forward our understanding of the disease, and target interventions towards the most vulnerable.
UNDP’s Work on Human Rights, Key Populations and Gender
UNDP is guided by several principles related to promotion of human rights in all of its work. These include: (1) Respect for and promotion of human rights and gender equality as set out in the United Nations Charter, the Universal Declaration of Human Rights and other international treaties, and (2) Meaningful engagement of people living with HIV, key populations, other excluded groups and affected communities is essential for effective health policy, programming and governance.
As a founding co-sponsor of the Joint United Nations Programme on HIV/AIDS (UNAIDS), under the UNAIDS Division of Labour, UNDP is mandated to convene the work on removing punitive laws, policies, practices, stigma and discrimination that block effective responses to AIDS and to co-convene the work of HIV prevention among key populations together with the United Nations Population Fund (UNFPA) as well as efforts to increase investments and efficiency in the use of resources for HIV, jointly with the World Bank. UNDP also leads the follow-up work to the recommendations of the Global Commission on HIV and the Law and is represented on the Global Fund Human Rights Reference Group.
UNDP manifests its commitments to uphold and promote these principles in many ways, a number of which are highlighted in this text. UNDP has significant experience supporting design, implementation and evaluation of Global Fund programs to remove human rights and gender related barriers to accessing health services. For example, UNDP has served as the Principal Recipient (PR) for four Global Fund regional grants in South Asia, the Western Pacific, Africa, and the Caribbean. Each of these grants focuses on strengthening the legal and policy environment for key populations, challenging stigma and discrimination, and building community capacity to effectively address human rights and gender barriers to access to and uptake of HIV, TB and malaria services.
In addition, UNDP has significant experience implementing programs to support key populations. For instance,
Integrating Human Rights, Key Populations and Gender in the Grant Lifecycle
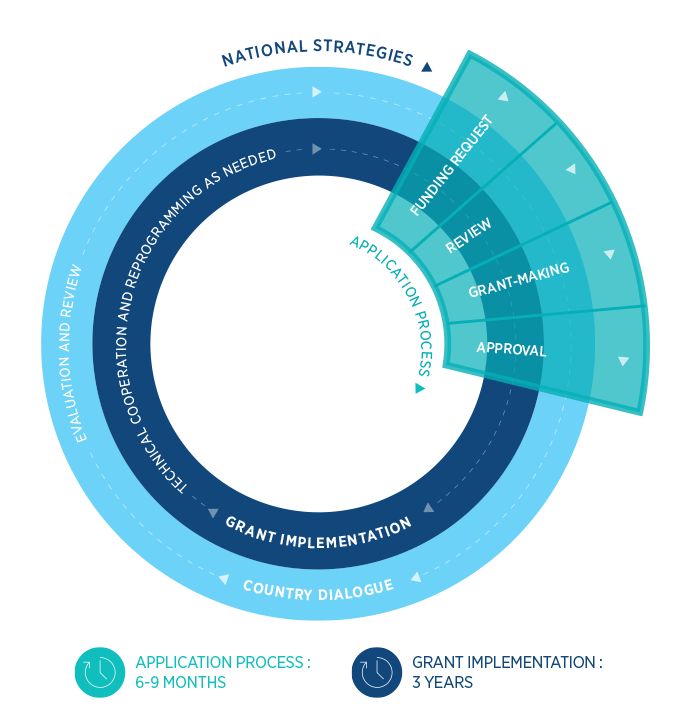
The guidance in this sub-section of the Manual is designed to guide UNDP’s efforts as Principal Recipient (PR) to strengthen the attention paid to gender, human rights and key populations in the implementation of programmes supported by the Global Fund, through the processes and mechanisms of the Global Fund’s funding model. Each stage of the funding model requires specific actions to address the dimensions most relevant for women and girls, key populations and other marginalized groups in the development and implementation of Global Fund grants.
The Global Fund is currently developing differentiated guidance for countries, which will impact the process by which countries access funding. The new guidance will be reflected in this document when it is available.
National Strategic Plans (NSPs)
The Global Fund bases its support on funding requests that are based on disease-specific NSPs that are robust, prioritized and costed. To serve as the basis for funding, the Global Fund expects NSPs and the national health strategy to be developed through inclusive, multi-stakeholder efforts (involving key populations), and be aligned with international norms and guidance. They should also be built on a clear understanding of the national epidemic based on epidemiological data disaggregated by age and sex, with specific analysis related to human rights, gender and key populations, and other barriers that affect access to health services.
- NSP analysis is conducted
- A needs assessment specific to gender, key populations and/or other marginalized groups, including a Legal Environment Assessment, is conducted
- The needs and rights of women and key populations are represented on the Country Coordinating Mechanism (CCM)
 Practice
Pointer
Practice
Pointer
- Despite focused efforts, it has been recognized that robust, prioritized and costed NSPs are often few and far between. Technical support and assistance is available from various donor agencies to either strengthen NSPs or to conduct the analysis needed for developing a strong funding request. UNDP has developed a roster of qualified consultants who will be available to support this process. In addition, the Global Fund will allow countries to reprogramme up to US$150,000 of funds from existing grants to support this work, if it is requested by the CCM.
- This should include efforts at ensuring that the epidemiological data which will normally inform the performance targets in the Country Grants are correct and realistic to avoid a situation where targets are based on incorrect data from poor size estimations and routine surveys. This has been the experience in a number of countries and has been responsible for the poor performance recorded in their Office of the Inspector General (OIG) assessment Report.
- A number of strong tools help guide a gender assessment. These include the UNAIDS Gender Assessment Tool ; as well as the forthcoming Gender Assessment Tool for HIV and TB co-infection.
Technical Assistance (TA) to support development or updating of NSPs is also available through a number of bilateral technical providers listed below, at every stage of the grant cycle:
- The United States President’s Emergency Plan for AIDS Relief
- Malaria support through Roll Back Malaria Partnership
- French 5% Initiative
- BACKUP Gesundheit – Support for partners in their work with the Global Fund
Country dialogue and funding request development
Country dialogue and funding request (previously called ‘concept note’) development are especially critical points during the grant cycle and present an opportunity to consult widely with a range of stakeholders—key population and women’s networks, networks of people living with HIV, communities, civil society, government, technical partners—to advocate for inclusion of activities to promote an enabling environment. These partners should ideally be involved at every stage of the grant cycle.
A wealth of guidance documents exist to support development of these interventions. The Global Fund HIV Information Note provides guidance to Global Fund applicants on employing strategic investment thinking when developing funding requests for HIV related programming. A thematic section on addressing human rights and gender related barriers is included. Similarly, The Global Fund Tuberculosis Information Note and The Global Fund Malaria Information Note include disease specific information and include sections on addressing rights and gender related barriers.
- Identify human rights barriers
Grant-Making
The performance framework (PF) for the Africa Regional grant includes good practice examples of indicators and workplan tracking measures related to removing legal barriers.
For more information on Workplan tracking measures (WPTM) and Impact/Outcome indicators, please refer to the Monitoring and Evaluation section of the Manual.
- Workplan tracking measures (WPTM) are qualitative milestones and/or input or process measures to measure evaluate progress over the grant implementation period for modules and interventions that cannot be measured with coverage or output indicators. This is most often the case in regional grants or grants that include modules related to, for example, community systems strengthening, certain health system strengthening interventions, removing legal barriers to access, activities addressing gender inequalities, health sector linkages, etc.
- Impact/Outcome indicators are often not available for inclusion in the PFs of regional grants that seek to exclusively to strengthen legal or policy environments, and community systems. However, impact and outcome indicators may be included for certain grants based on the grant’s objectives and in agreement with the Global Fund and the Principal Recipients (PR) (please confirm with your Global Fund Country Team).
- Programme reviews, assessments, or evaluations can serve an important role in assessing performance against grant objectives for grants where no standard indicators are available for use. These normally encompass grants that are focused on strengthening legal and policy environments and community systems. In these scenarios, the need and scope of an evaluation, assessment, and/or thematic review should be agreed with the Global Fund and Principal Recipients (PR). Country Offices (COs) are also encourage to consultant with GFPHST and the GF CT to ensure that adequate budgets are allocated to fund agreed studies (for an evaluation both baseline and endline must be covered). More guidance on measuring equity, gender equality and human rights is here.
 Practice
Pointer
Practice
Pointer
- For WPTM, ensure concrete, measurable actions at a process level that also contribute to a meaningful assessment of progress. For example, instead of measuring whether meetings to discuss the treatment cascade for KPs occurred, measure who attended, whether minutes with concrete next steps were produced, etc.
- Do not overcommit – ambitious and realistic expectations must be balanced, so it is recommended to keep the number of WPTM to a minimum; ‘less is more’
- Sex- and age-disaggregated data is a key feature for gender-sensitive and/or transformative programming, as it helps to identify key populations and address their needs appropriately by introducing gender-sensitive investments, creating an appropriate national response to the elimination of the three diseases.
 Practice
Pointer
Practice
Pointer
- It is critical to ensure that the advocacy to include enabling environment interventions in the funding request is not lost at the time of grant-making (and during implementation). Ensure interventions in the funding request are included in the detailed budget at adequate levels, including sufficient funds for evaluations at baseline, midterm and endline as appropriate for the programme. This often requires skilful negotiation with the Country Coordinating Mechanism (CCM) and Global Fund to understand the importance of these interventions within the context of the grant.
- At times Global Fund finance staff may not have a background in budgeting for human rights, and therefore may not fully understand the budgeting implications for human rights. interventions within the overall context of a grant. For example, the Global Fund may request reductions in human resources to implement certain activities, or deprioritization/omission of enabling environment activities if overall grant funds have been reduced. In this case, robust explanations including job descriptions and evidence from various sources cited throughout this section should be provided in order to justify the inclusion of these interventions.
Grant Implementation
Once the Global Fund grant has been signed and a disbursement has been received, some Programme Managers have expressed concern that there is insufficient capacity in the Project Management Unit (PMU) to effectively deliver on human rights and gender programmes. This risk can be mitigated by ensuring proper planning and involvement of CSOs and consultants, preferably engaged from programme design and inception, with the requisite knowledge and experience to implement programmes.
 Practice
Pointer
Practice
Pointer
- Reprogramming: In consultation with your Programme Advisor in the UNDP Global Fund Partnership and Health Systems Team (GFPHST), as well as jointly with Sub-recipients (SRs), Programme Managers are encouraged to identify areas for which savings can be used to scale up/reprogramme funds, based on recommended programming included in the Global Fund Human Rights Information Note, and the UNAIDS key programmes to fight stigma and discrimination (scale up of trainings/desensitization for health care workers; anti-stigma and discrimination advertisements, Legal Environment Assessments (LEAs) etc.).
- Technical support:Engage with CSOs and key population and women’s networks early to support implementation/provide TA.
- Early warning: It is important to identify issues early. For example, if activities are not implemented due to sensitivities, lack of attendance, Country Coordinating Mechanism (CCM) “politics”; human resource constraints or capacity, etc. contact your UNDPGFPHST Programme Advisor for support and guidance.
- Communication efforts: It is important to ensure that programme activities are communicated to relevant stakeholders including the Global Fund and other donors, as a viable source of advocacy for future funding of these programmes. Modalities employed can include Newsletters, Facebook, Twitter, and impact sheets that highlight key activities and results. The Multi-country Western Pacific integrated HIV/TB programme website and the Africa Regional grant on HIV website include good examples of communication efforts.
- Appoint a country ‘high-level champion’ to advocate for consistent attention to the gender, key population and human rights dimensions of the three diseases.
Access to Medicines
Access to affordable medicines, diagnostics, vaccines and other health technologies of good quality is an essential component of the right to health and the right to the benefits of scientific progress. It is a core obligation of countries to provide essential medicines as defined by WHO.
The UNDP, WHO and University of Oxford Global Dashboard for Vaccine Equity shows that COVID-19 vaccine inequity will have a lasting and profound impact on socio-economic recovery in LMICs. The COVID-19 pandemic gaps in equitable access extend beyond vaccines and include other health technologies such as diagnostics and treatments.
Responses to pandemics and other health priorities can be hindered by national and regional laws and policies that may not support or are, in fact, contradictory to the goal of ensuring rapid innovation, access and delivery of health technologies. On the other hand, well-designed policies and laws can help to build and sustain systems to address and manage the pandemic prevention and response and Universal Health Coverage, and can complement and reinforce global efforts to increase equitable access to diagnostics, vaccines, and treatments.
There has been a long-standing recognition of the need for coherent policy and legal frameworks that support equitable access to health technologies. The Global Commission on HIV and the Law, and the UN Secretary General’s High-Level Panel on Access to Medicines are two global independent bodies that evaluated lessons learned and recommended the creation of coherent legal and policy strategies to advance access to health technologies
UNDP support countries in the strengthening of capacities that promote policy coherence and create enabling legal and policy environments that promote access to medicines and other health technologies. In addition to technical assistance and capacity building at country request, UNDP aims at thought and strategic leadership in this area of work – through development of guidance documents and other knowledge products as resources for use by government stakeholders, development partners and civil society.
Examples of country support include the following:
- UNDP partnered with the government of Kazakhstan, through a project supported by the World Bank in developing a national Intellectual Property strategy and crafting strategic approaches to intellectual property protection, which incorporated the TRIPS flexibilities also to facilitate access to medicines and health technologies. The Law of Kazakhstan on patents was amended in June 2022, adopting the key approaches proposed in the national IP strategy, including limiting the scope of people and organizations that can be patent representatives, capping the opportunities for extension of petty patents, excluding diagnostic methods, methods of human cloning and clones, methods for altering the genetic integrity of human cells from patentability, introducing rules for invalidation of Eurasian patents.
- In Malawi, UNDP has supported the government technical working group tasked with the review of the national patent law, identified as a key follow up to the high-level regional meeting on policy coherence in the ARIPO region for access to health technologies in late 2017.
- In Malawi and Uganda, UNDP recently initiated a project aimed at increasing access to treatment and care for people living with diabetes and other NCDs. The project will help develop and implement Legal Environment Assessments (LEAs) that will help drive evidenced-based government decision-making on access to treatment and care.
- In Namibia, UNDP has worked with the government in the amendment and implementation of the national competition law to increase access to medicines.
The COVID-19 pandemic has highlighted increasing inequities in the access to a range of health technologies for an effective pandemic response. A diverse toolkit of legal and policy interventions is needed to increase access. Interventions aimed at strengthening the access and delivery value chain at the national level are crucial to address the capacity gaps for rapid approval and delivery. There is also increasing focus on technology transfer and local production of health technologies as means of increasing access. UNDP plays an active role within global initiatives aimed at facilitating effective technology transfer and local production, as well as supporting government efforts. For example, since 2019, UNDP has provided technical assistance and support to the Ministry of Investment, Industry and Trade (MIIT) in Tanzania in its efforts to developing a national strategy aimed at promoting the development of the domestic pharmaceutical sector.
